Trauma to the nose: When is surgery the right choice?
Trauma to the nose: When is surgery the right choice?
Experiencing trauma to the nose can be an alarming event. Given its prominent position, the nose is highly vulnerable to injury from falls, sports, or accidents. While immediate pain and swelling are universal, the critical question is whether this injury requires specialist surgical attention.
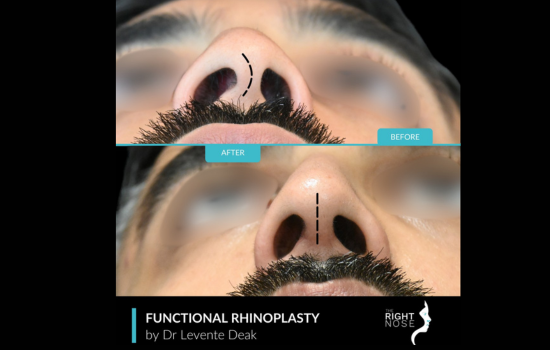
Dr Levente Deak’s practice focuses entirely on nasal surgery, meaning he approaches every nasal trauma case to restore the airway (function) and preserve facial harmony (aesthetics).
Understanding when to monitor a minor broken nose and when to commit to functional rhinoplasty is essential for achieving the best long-term outcomes.
Assessing the damage: Broken vs Swollen
How to know if your nose is broken or just swollen?
The most common immediate concern is whether your nose is broken or swollen. Significant swelling can obscure the underlying structure, making an initial self-assessment difficult. However, there are key indicators that suggest a severe nasal fracture (a broken nose) has occurred:
Obvious deformity: The nose appears visibly crooked, flattened, or shifted to one side. The bones are likely displaced if the crookedness persists after the first few hours of injury.
Severe, localised pain: Pain that is intense and localised to the bridge of the nose, often accompanied by a crunching or grinding sensation upon light touch.
Breathing difficulty: Persistent inability to breathe through one or both nostrils, especially after the initial, general swelling subsides (usually within 24 hours).
Black eyes and bruising: Extensive bruising that spreads rapidly to the eyes. Even in cases of a minor broken nose where displacement is minimal, an evaluation is crucial.
A simple fracture can hide a septal hematoma (a blood clot in the septum), which requires immediate drainage to prevent severe damage to the cartilage.
The critical role of cartilage and long-term symptoms
Many people focus only on the nasal bones, but the nose’s support system is largely made of cartilage.
Damage to the cartilage, particularly the nasal septum, is often the most critical injury, dictating the need for surgery.
Broken nose cartilage symptoms include the tip of the nose losing its projection and appearing to collapse or droop downward.
- Saddle nose deformity: The mid-section of the nose sinks, creating a dip or ‘saddle’ shape resulting from the loss of septal cartilage support.
- Nasal valve collapse: Upon inhalation, the internal structures of the side walls of the nose collapse, severely restricting airflow.
If significant cartilage damage is left untreated, the long-term symptoms of a broken nose will inevitably manifest, typically as a chronic, frustrating inability to breathe through the nose.
This structural failure can lead to a collapsed nasal structure, making the nose ineffective at filtering and warming air, causing sleep disruption and chronic sinus issues.
While broken nose cartilage healing time can take many months to achieve structural stability, prompt intervention is necessary to set the foundation for that healing.
The surgical decision: Functional rhinoplasty
When severe trauma results in significant displacement, visible deformity, or breathing obstruction, surgery is the right choice. The timing of this surgery is critical and usually falls into two distinct categories:
Acute reduction (Within 7-14 days): A closed reconstruction can be performed for simple fractures where the bones are displaced but the soft tissues are still pliable.
This is done by manipulating the bones back into alignment under anaesthesia. This early intervention is straightforward and prevents the need for major surgery later.
Delayed functional rhinoplasty (6-12 Months): If the initial injury was missed, ignored, or resulted in complex cartilage destruction that was not fully addressed, the final correction is achieved through functional rhinoplasty. This advanced surgical technique is designed to correct the deep architectural damage.
It involves rebuilding the septal and lateral cartilage supports to repair a collapsed nasal structure and open the internal valves. By prioritising internal function, we can correct external crookedness and post-traumatic deformity.
Delaying this final surgery allows all swelling to completely resolve, giving me a clear, stable view of the actual, underlying post-traumatic deformity.
Choosing a surgeon with specific expertise in functional rhinoplasty post-trauma is paramount. The goal is cosmetic refinement and the meticulous repair of the nasal airway, ensuring the nose works as nature intended. If you have suffered trauma to the nose, it is essential to seek a timely consultation.
The difference between a simple, acute reduction and a complex, delayed reconstruction can depend entirely on seeking expert advice within the first few days of the injury.
Take the first step toward healing
If you’ve recently suffered nasal trauma, don’t wait until minor issues become long-term complications.
Dr Levente Deak specialises exclusively in nasal surgery, combining advanced surgical skill with a deep understanding of function and aesthetics.
Dr Levente Deak is a Consultant ENT and Facial Plastic Surgeon, distinguished as a European Board-Certified ENT Surgeon and a USA and EU Dual Board-Certified Facial Plastic Surgeon.
He is an authority on nose and face correction procedures, with over 15 years of experience focused exclusively on the face, emphasising Rhinoplasty, Blepharoplasty, and Nasal Airway Correction.
He is a member of the European Academy of Facial Plastic Surgery (EAFPS). Schedule your consultation today and ensure your recovery is guided by expertise, precision, and care.
Some Quick FAQs
Your nose likely requires surgery if you have persistent, severe difficulty breathing through one or both nostrils, if the nose remains visibly crooked or deformed after the initial swelling has reduced (3-5 days), or if a septal hematoma is diagnosed.
A nose injury is considered serious if there is profuse, uncontrolled bleeding, drainage of clear, watery fluid (which may indicate a leak of cerebrospinal fluid), rapid and significant swelling that blocks both nostrils, or a severe, visible change in the shape of the nose.
Initial swelling typically subsides within the first 7 to 14 days. After 4 to 6 weeks, the nasal bones and cartilage are generally stable enough for light activity. However, complete healing, including the full resolution of all internal swelling, takes at least six months and often up to a full year.
If a fracture is displaced, the ideal window for a simple closed reduction is within 7 to 14 days of the injury.
For chronic breathing issues or cosmetic deformities that persist after the injury, functional rhinoplasty is typically performed 6 to 12 months after the trauma to ensure all swelling has resolved and the final, stable deformity can be accurately corrected.
Damage to the nose can result in a simple bruise, a fracture of the nasal bones, a severe deviation of the septum (the internal wall of cartilage), or a collapse of the internal support structures. Untreated damage often leads to chronic nasal obstruction, persistent cosmetic deformity, and occasional nosebleeds.